For a lot of patients, taking medications as prescribed is a harder proposition than simply following the directions on the side of the bottle.
Up to 80% of patients drop out of chronic care management plans, according to research published in the Journal of Medical Internet Research. This has a knock-on effect on the quality of the care they receive, as well as costs. Non-adherence to medication instructions results in up to 125,000 deaths, at least 10% of hospitalizations and around $300 billion in medical expenses annually, according to a review from the Annals of Internal Medicine.
Furthermore, previous studies have shown that between 20% and 30% of prescriptions go unfilled and about 50% of chronic disease medications are not taken as prescribed. This has a major impact on the ability of medications to perform in a way that matches results found in clinical trials. As former Surgeon General C. Everett Koop told the New York Times in 2017, “Drugs don’t work in patients who don’t take them.”
Health IT to the Rescue?
IT solutions are often bandied about in conversations about addressing inefficiencies and cost centers in any business. The case of healthcare’s medication adherence problem is no different. However, there is no out-of-the-box solution or single application that can simply change habits or address issues related to social determinants of health (SDoH).
But technology can help healthcare professionals attack the problem from a number of angles. The first step, according to an article from the New England Journal of Medicine, is understanding three important processes in adherence: Initiation, implementation and discontinuation.
Initiation refers to the patient taking their first dose. Implementation is a measure of how well the patient follows the prescribed dosing regimen, while discontinuation refers to when the patient stops taking the medication, regardless of whether they were instructed to or not.
There are a range of factors that impact each process, from social or economic factors to patient related, therapy related, condition related or healthcare system related factors.
Possible Technology Solutions
Solutions then, have to address each process through the lens of these factors. An example in the initiation phase is failure to fill a prescription. Reasons for this may involve a fear of side effects or not understanding why the medication was prescribed to begin with. Applications focused on patient education regarding why they’ve been prescribed certain treatments, the health consequences of not adhering, the possible side effects and food-drug interactions could prove helpful.
Some applications are even encouraging patients to keep a diary or invite family or care team members to view their progress so they can help hold the patient accountable. In the case of Mango Health, users earn points for taking their medication. If they earn enough points, they can win prizes, thus gamifying the activity to create an incentive for adherence.
When it comes to implementation, a common example is patients simply not remembering to take their medication on the prescribed schedule.
There are a number of applications that provide medication scheduling and notifications. Some provide a text message reminding the patient to take their meds while others, such as DoseCast take a more proactive approach, listing all of a patient’s medication and organizing them by prescribing physician while also notifying the patient regardless of internet connection and providing time zone tracking so the patient receives notifications at the right time no matter where they are.
DoseCast also uses multiple alert tones and signals to remind patients of their schedules, a feature that can come in handy for patients taking 13 or more medications per day. That population experiences a 20% adherence rate, according to a study published in the journal Therapeutics and Clinical Risk Management.
Finally, there are issues related to discontinuation. A major cause of discontinuation is maintaining a prescription refill schedule and patients understanding the importance of long-term medication use. For those with chronic conditions, this is particularly important.
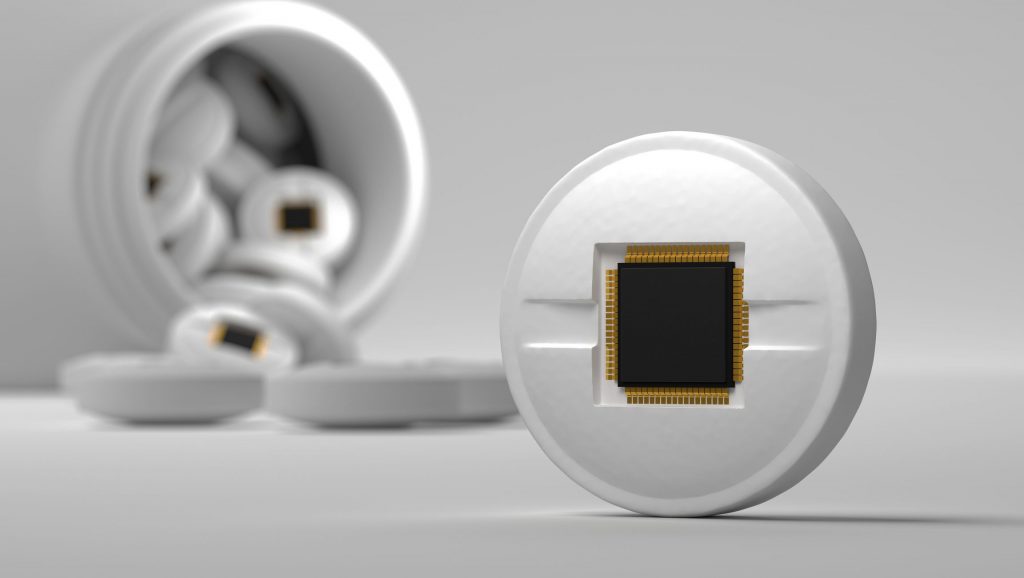
Applications aimed at this process include smart pill bottles and even digitizing the pills themselves so that providers can track patients taking their medication and pharmacies can be alerted when the patient runs out of medication. Another example comes in the form of MediSafe Meds and Pills Reminder, which can create alert tones that sound like famous characters such as Darth Vader or Austin Powers to tell you to take or refill your meds.
Adherence and Organization
A major problem with adherence is simply keeping medications organized. According to a survey conducted by Consumer Reports, 53% of all people who take prescription medications take more than one of them. This is to say nothing of over-the-counter drugs, vitamins and supplements. Keeping all of these dosages organized is a task generally left up to the patient, using things such as pill organizers. But even those require maintenance and a certain level of dedication.
Efforts in medication synchronization, the practice of coordinating refills so that all of a patient’s medications can be picked up on a single day, are leading to a higher level of patient engagement for pharmacists. Getting a patient to buy in to medication synchronization puts all the data in front of a pharmacist at once and allows the pharmacist to easily schedule consultations that can lead to higher satisfaction for both parties and help identify barriers to adherence.
This is now being taken a step further by improving packaging options. While synchronization may improve patient willingness to refill prescriptions on time and to consult with a pharmacist, it still leaves issues with someone who takes multiple medications keeping them all organized. Now, some pharmacies are experimenting with the packaging, organizing all of a patient’s medication into a single serving pouch so that patients simply take their meds simultaneously according to the schedule.
According to a study published in Innovations in Pharmacy, blister or bubble packaging significantly improves the level of adherence, particularly when paired with medication therapy management sessions. Another idea with blister or bubble packaging to encourage adherence includes placing a phone number inside the packaging that the patient must call to verify they took their medication.
Enter health IT, with ingestible sensor technology and smart bottles that can detect when the bottle is opened and a pill removed. Enter applications that allow for users to log their compliance with prescription instructions by taking a picture of their meds and themselves taking it. All of these solutions have potential in helping address adherence issues through a more modern approach.
And now, perhaps some of the most fascinating potential health IT solutions include wearable sensors that indicate whether someone has swallowed their medication. This comes in the form of a “smart necklace” according to research published in the journal Artificial Intelligence in Medicine, which reports that the necklace can “correctly classify between chewable vitamins, saliva swallows, medication capsules, speaking, and drinking water, with average precision and recall of 90.17% and 88.9%, respectively.”
Involving Healthcare Providers in the Process
While all these ideas have merit and sound good on the surface, direct involvement of healthcare professionals in their development is lacking, according to a study published in JMIR mHealth uHealth.
The study looked at 5,881 adherence applications, separating them by whether they cost money or were free and whether they tied healthcare professionals into the development of the app. They concluded: “The results demonstrate a concerning lack of healthcare professional involvement in app development and evidence base of effectiveness. More collaboration is required between relevant stakeholders to ensure development of high quality and relevant adherence apps with well-powered and robust clinical trials investigating the effectiveness of these interventions.”
Healthcare’s complexity and the compliance environment require heightened knowledge of industry regulations and practice in app development. Healthcare and pharmaceutical professionals who can bridge the gap between understanding technology systems and data collection and how they will best fit into the spectrum of care, provider workflows and patient engagement efforts are likely to find success.