Healthcare faces many challenges as leaders attempt to improve patient care, reduce costs and implement technology into both clinical and business processes. Increasingly, leaders are seeing they can benefit from using continuous process improvement.
However, as popular as Agile is as a process improvement methodology, it hasn’t made its way into healthcare like it has other sectors. Only 30% of healthcare executives are familiar with Agile according to consultants Bain & Company. However, 75% of those who do implement Agile say their teams perform better or significantly better than traditional teams.
Bain & Company writes that “even previously skeptical healthcare and life sciences executives are using Agile teams to unleash a powerful burst of innovation.”
What is Agile?
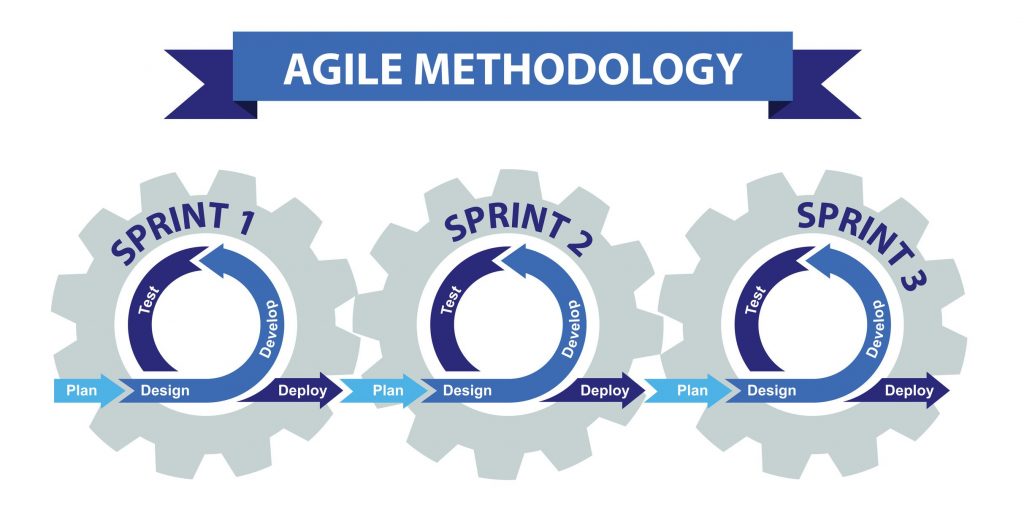
Invented for the software industry, Agile was created to speed up the development process while also maintaining the quality of the product. Rather than relying on legacy processes that often led to long delays, Agile emphasizes getting a product done quickly through short sprints and using end-user feedback to make improvements.
The Agile Manifesto originally written by software developers focuses on the following values:
- Individuals and interactions over processes and tools
- Functional software over extensive documentation
- Teamwork with customers over contract negotiation
- Responding to change over following a plan
Healthcare, which in many cases has been locked into systems that are decades old, is particularly ripe for the use of Agile.
The Need for Process Improvement in Healthcare
Healthcare administrators are under pressure to create more efficient health systems while also improving patient outcomes. But making big changes in a long-established industry can be like turning around the Titanic. It’s going to take some time.
Agile is designed to speed up that process. Most healthcare providers are now trying to create processes that align with what is called the Triple Aim initiative. It starts with the individual patient experience in terms of cost and the benefits of treatment, and then extrapolating that to create new approaches for patient populations as a whole.
This is another distinguishing characteristic of Agile. Much like Lean Six Sigma, another process improvement methodology, Agile requires that organizations focus on evaluating every process and decision through the lens of whether it benefits customers.
Agile revolves around iterative development, which calls for taking a larger process and breaking it into small chunks. A project team focuses on these smaller chunks in what are known as “sprints,” using focused “scrum” meetings to quickly brainstorm and create solutions to challenges.
The emphasis is on moving as fast as possible toward a solution without sacrificing quality – but also recognizing that perfection cannot be attained and that feedback from users will lead to improvements in future iterations.
Should Healthcare Adopt Agile?
The decision on whether to adopt Agile revolves around the nature of the problem itself. However, some form of Agile can be applied to most situations.
Agile works best with processes that are central to what healthcare administrators want to accomplish. Areas include:
- Patient experience
- Clinical workflows
- Implementing digital health technology
Any of the above can help healthcare leaders provide better levels of patient care. They also can provide the opportunity to learn about patient experience and the costs for treatment.
Agile works best if there is a measurable goal to be reached. For example, reducing the number of patient bed calls made to nurses during the overnight shift. Or reducing the number of Medicaid claims denials within a given period.
The best practice is to start with the goal (which should involve a benefit to patients) and then working toward finding the best path to accomplishing that goal.
Can Agile Improve Healthcare Innovation?
The whole point of Agile is to improve innovation. However, as with other industries, it only can work in healthcare if senior management has complete buy-in to the process, as pointed out by Health Affairs.
Some have put Agile into action. For example, Health Affairs reports that Inception Health was started to “accelerate innovation through more rapid cycle project management, contracting, and dedicated investment for innovation.”
Inception Health works with medical providers in Wisconsin health networks to develop solutions to process improvement challenges.
There is a still a long way to go in implementing Agile, as the lack of awareness of the methodology in the Bain survey showed. But for those moving into the healthcare field, it’s reasonable to expect that process improvement methodologies such as Agile will be part of the job in the future.